Press Briefing on National Strategy for Pandemic Influenza Implementation Plan One Year Summary
Room 450
Eisenhower Executive Office Building
PARTICIPANTS:
Dr. Rajeev Venkayya, Special Assistant to the President for Biodefense
Ambassador John Lange, State Department Special Representative on Avian and Pandemic Influenza
Dr. John Clifford, USDA Chief Veterinarian
Admiral John Agwunobi, Assistant Secretary of Health
Dr. Jeff Runge, DHS Chief Medical Officer on Pandemic Preparedness
1:02 P.M. EDT
MS. BERGMAN: Good afternoon, everyone. Thank you very much for coming to today''s session. I want to welcome you to our discussion of the first year of implementation of the National Strategy for Pandemic Influenza. And a quick word about the logistics of today''s briefing. We will begin the briefing with remarks from Dr. Rajeev Venkayya, Special Assistant to the President for Biodefense. From the State Department we have Ambassador John Lange, Special Representative on Avian and Pandemic Influenza. From USDA, we have Dr. John Clifford, USDA Chief Veterinarian. From HHS, we have Admiral John Agwunobi, Assistant Secretary of Health. And from DHS, we have Dr. Jeff Runge, Chief Medical Officer.
I want to remind you that today''s briefing is on the record. And for members of the media who are here in attendance, I request that you wait until the conclusion of the stakeholder briefing and ask your questions at that time. The participants will stick around for media questions after the stakeholder briefing. Thank you.
And with that, I will turn it over to Dr. Venkayya.
DR. VENKAYYA: Thank you, Cynthia. And I want to thank all of you for joining us today. We wanted to take this opportunity on or around the one-year anniversary of the implementation plan of the National Strategy for Pandemic Influenza to summarize our progress.
You will have received or had access to a glossy narrative report of our progress that was available outside. That document will be made available over the web at pandemicflu.gov, and we anticipate that being on the White House website, as well. There''s also a blow-by-blow, action-by-action report similar to the one that we released in December around the six-month time frame that describes our assessment as to where we are in each one of the actions that was due to be completed within 12 months.
Just to quickly recap what events brought us here, back in November, as I think many of you are aware, the President released the -- November of 2005 -- the President released the National Strategy for Pandemic Influenza, largely to highlight the need to transform this from an animal health and human health issue to a national priority -- a national security priority, a national health priority, a national economic priority.
In addition to doing that domestically, we did that internationally. We established the International Partnership on Avian and Pandemic Influenza, and the Department of State has led an aggressive effort to engage our international partners to further emphasize the importance of addressing this pandemic threat.
The strategy is a very high-level document. It lays out the principles that guide our international efforts. The implementation plan released in May of last year provides over 300 actions that direct federal departments and agencies to act in the name of the principals in the strategy itself. Each of those has a measure of performance and a timeline for completion, hence the report at one year. We''re basically cataloguing our progress on those 12-month actions.
Before I turn to my colleagues, I''d like to just quickly run through the reason why we''re concerned about the H5N1 threat. As I think many of you are aware, we began back in 2005 with a recognition that this new influenza virus had been documented in about 16 countries globally. Since that time, the number of countries with documented bird infections of H5N1 has increased to 60.
And so this outbreak in birds does not show any sign of abating, but more concerning -- of greater concern is the fact that we know that this virus can infect humans. And although it hasn''t infected many humans, to our knowledge -- right around 300 individuals worldwide -- the mortality in those that it has infected is right around 60 percent.
Now, why is this important? Well, we''ve faced three pandemics in the last century; we face influenza pandemics on a regular basis, about three every century for the past several. And the most serious of those in the 20th century killed about 20 to 40 million individuals worldwide, and that was with a mortality rate of 1 to 2 percent.
We don''t know what''s going to happen with this particular influenza virus, but if it''s not H5N1, we can be certain that some other influenza virus at some point in the future will lead to a pandemic. More importantly, if it''s not an influenza pandemic in the next 10 years, we know -- we can almost be certain that some other biological threat will come upon us and we will need to be prepared for that.
Now, the media''s attention has waned a bit, and the public''s attention has waned a bit to this threat, and there are understandable reasons for that. But it''s important for governments and officials at the federal, state and local level, as well as those who are in charge of companies, non-governmental organizations, churches, other faith-based organizations, and individuals to keep this in mind, because this preparedness effort that we''ve undertaken is not done. We had a huge gap ahead of us when we started this in 2005; we still have a very sizeable gap in front of us.
So there is much work that needs to be done, and we need to continue to take this -- take advantage of the time that we have.
Let me turn now to the report that''s being released today. Of the actions that were due at 12 months, we assess that 86 percent of those actions have been completed. That''s to be compared to a score of around 92 percent that we released at the six-month mark. There are about 14 percent of the actions that are not yet completed. We document those in the action-by-action detailed report. We anticipate those being completed in the 18-month time frame at the next six-month report.
I''m not going to go through the accomplishments in great detail. Suffice it to say that on the international front, we''ve taken unprecedented action. We have committed more resources to this problem than any other country in the world. Our contribution to international efforts numbers about 20 percent of all global contributions to avian and pandemic influenza efforts. Here domestically, the USDA and Department of Interior have launched a phenomenal surveillance program. You''ve seen the outputs of that. We found lots of low-path avian influenza. And it''s good news that it''s low-path. It''s also good news that it, I think, validates, to some degree, our wild bird and domestic bird surveillance activities.
On the human health front, we''ve embarked on a moon-shot approach to reestablishing vaccine production capacity and new technologies such as adjuvants to stretch the effectiveness or the number of individuals we could vaccinate with a single dose of vaccine. Admiral Agwunobi will speak more about that. He will also speak about the community mitigation guidance that was released by Dr. Gerberding in February, which essentially provides a road map, an essential road map, we think, for communities, in light of the hard, cold facts, and that is that we are almost certainly not going to have sufficient health and medical capacity to take care of the large numbers of individuals that would be presented by a several pandemic.
I think it''s also important to point out that there are certain things, certain policy issues that we''ve addressed in the past year, really tough things that we, as a government, have grappled with. This, by the way, has led to us postponing a handful of actions, postponing the deadline, if you will. I''ll just highlight a couple of them.
One is the critical question of what we''re going to do at our borders during a pandemic. I think many people on this stage get asked that question whenever they speak about pandemic flu. The question is, will we close the borders? And some people say -- if we say no, some people say why not, and if we say that -- in other words, the thinking being that if you''ve got a biological threat, why wouldn''t you seal your borders?
The reality is that there are tremendous challenges to sealing our borders to begin with. Secondly, we believe, and scientists concur, that if a pandemic virus emerges anywhere on the globe, it is inevitable that it will arrive here in the U.S., irrespective of the actions that we take at the borders.
And so our planning approach is to plan to limit the arrival of individuals who might be affected with a pandemic virus, those who might be affected to place them -- to give public health -- implement public health measures to limit onward transmission, but to do what we can to also simultaneously preserve the flow of goods and people.
Another policy issue that we''ve grappled with is vaccine prioritization: In the setting of insufficient vaccine, who should get vaccine first? The reality is that there''s not going to be a single answer. It will depend upon the characteristics of the pandemic -- the population, the age group that the pandemic virus seems to favor, as well as our supply, as well as the overall impact we anticipate on our national infrastructure. And so the Department of Health and Human Services and Homeland Security have worked with public groups, professional societies and others to develop a draft of that prioritization guidance that you can anticipate seeing in the coming weeks for public comment.
Despite all the progress that''s been made, in closing I just want to highlight that we do, in fact, have a lot of work ahead. A couple of items that I''d point to are our surveillance capacity, both internationally and domestically. We continue to have a great deal of difficulty in determining when outbreaks of infection occur in animals and in humans overseas. Just to be brutally honest, we have a lot of trouble determining when we have an outbreak of infectious disease in a community here in the United States. We have limited surveillance capability here in the U.S.
Now, CDC has led tremendous efforts to enhance that, and there have been remarkable efforts in many localities to enhance that surveillance capability. But we need to have uniform biosurveillance capability, we believe, to prepare us not only for a pandemic but any outbreak of infectious disease. We need to further enhance our mass casualty care capabilities in communities, referencing back to the point that I made about insufficient bed space and public health capacity. We need to implement the community mitigation road map that''s been laid out by the CDC. And then finally we need to attend to a concern that''s been highlighted for us by countries that don''t have access to vaccine or don''t have much hope of having access to vaccine in the near future, and that is the issue of global vaccine access and a more equitable distribution of the life-saving countermeasures to the international community. And we are committed to working with the WHO and our international partners to address that.
So with that, I will stop. That was a long overview. What I''d like to do now is turn things over to Ambassador John Lange from the Department of State to give us first an overview of international activities.
Ambassador Lange.
AMBASSADOR LANGE: Thank you, Rajeev. Good afternoon. I''m pleased to be with you here today to talk about the U.S. government''s international activities related to avian and pandemic influenza.
Of course, infectious diseases know no borders. And a key aspect of our campaign to contain the spread of highly pathogenic avian influenza and to prepare for the possibility of a human pandemic is large-scale global engagement that has unfolded since the seriousness of the threat became apparent a few years ago -- specifically ongoing efforts by governments, international organizations, and the private sector.
In September 2005, President Bush announced the International Partnership on Avian and Pandemic Influenza. And the goals of the international partnership are to elevate avian and pandemic influenza on national agendas in governments around the world; to coordinate efforts among donors and affected nations; to mobilize and leverage resources; to increase transparency in disease reporting and improving surveillance, a point that Dr. Venkayya made about the importance of surveillance; and to build local capacity to identify, contain and respond to an influenza pandemic.
As many of you know, the international partnership convened in Washington in 2005, in Vienna, Austria, in 2006, and it will meet again in New Delhi, India, in December 2007. The Under Secretary of State for Democracy and Global Affairs Paula Dobriansky leads interagency delegations at each of these meetings.
There have been some other political-level international conferences in Beijing, China, and Bamako, Mali, that took place in 2006. Well over 100 nations and 20 international and regional organizations have participated in these events. And at these events, donor governments and the multilateral development banks and international financial institutions have really stepped forward, and the total pledges, as of last December, the last pledging conference, were $2.3 billion. The United States has made the largest pledge of any country, totaling $434 million, by the end of last year, and we anticipate further commitments will be forthcoming this year.
In sum, the world has been engaged and continues to be engaged on avian and pandemic influenza. This global engagement involves a really enormous, multi-faceted effort.
In the United States, as Dr. Venkayya mentioned, the Department of State coordinates the U.S. government''s international efforts, along the lines of the three pillars that are in the National Implementation Plan that was released in May of last year: preparedness and communication, surveillance and detection, and response and containment.
These international efforts, while coordinated by the Department of State, are really an interagency enterprise, including the agencies that are up here with me today. It involves not only the State Department but the Department of Agriculture, the Department of Health and Human Services, the Department of Homeland Security, Department of Defense, our major international assistance through the U.S. Agency for International Development, and various other federal entities all working internationally.
In terms of international organizations, we have cooperated very closely with the United Nations System Influenza Coordinator, Dr. David Nabarro, and with the institutions internationally who are very focused on programmatic activities in line with the concerns -- the Food and Agriculture Organization of the United Nations, and the World Organization for Animal Health, known as OIE by its French initials, are focusing on the animal health side; the World Health Organization on the human health side. And then there''s the World Bank and many other multilateral institutions.
And they''ve really all been engaged in actions in light of the alarming spread of the avian influenza virus in poultry, as Dr. Venkayya mentioned, now in 60 countries, as well as the possibility that there will be this global pandemic.
So what has this global engagement meant, in terms of specific accomplishments, as well as actions planned for the near future? I know there isn''t a lot of time available for this so I''ll just mention a few. And you, of course, have the results that have been printed today in the progress report.
The United States is supporting preparedness efforts in more than 65 countries, working in collaboration with WHO, FAO, OIE and other partners. We''ve deployed scientists, veterinarians, public health experts, physicians, emergency response teams, all to either affected or high-risk countries, to assist in the development and implementation of emergency preparedness plans relevant to both avian influenza and to pandemic influenza.
With our neighbors Canada and Mexico, we''re finalizing an avian and pandemic influenza plan that will be issued next month as part of the Security and Prosperity Partnership of North America. And this plan will lay out a sound, coordinated trilateral approach to prepare for and respond to the possibility of the arrival on this continent of highly pathogenic avian influenza, possibly in migratory birds or in poultry, or a human influenza pandemic.
We''re supporting activities in more than 50 countries to generate public awareness about the threat of avian influenza and to promote behaviors that reduce the risk of disease transmission from poultry to people.
We''re also providing up-to-date information on avian and pandemic influenza to the majority of over 2 million Americans registered with our embassies and consulates abroad by using websites, town hall meetings hosted by our embassies and consulates, publications and other means.
We''ve supported efforts to expand and enhance animal and human disease surveillance systems, and we''re working with partners to improve capacity for detection and laboratory diagnoses, as well as early warning networks in 75 countries.
With WHO and FAO, we''ve provided training for thousands of policy and technical experts globally who will lead efforts to contain and mitigate the effect of animal and pandemic outbreaks.
And to prepare for this, we did this -- total on this, we''ve supported the training of more than 129,000 animal health workers and 17,000 human health workers in surveillance and response.
This is only a partial accounting, and it''s very much done by a multitude of U.S. government agencies acting internationally. We''re going to continue that global engagement, and in particular, we look forward to the next meeting of the International Partnership on Avian and Pandemic Influenza in India this December.
Thank you.
DR. VENKAYYA: Thanks, Dr. Lange. I''d like to now turn it over to Dr. John Clifford from the Department of Agriculture.
DR. CLIFFORD: Thanks, Dr. Venkayya. I appreciate the opportunity to report on USDA''s progress in protecting against and preparing for highly pathogenic H5N1 avian influenza. We have worked very hard to ensure that we have an aggressive, thorough and detailed response plan in the event of a detection of a high-path, H5N1.
We''ve also worked very hard in an international basis to prevent the spread of high-path H5N1 overseas, thereby better protecting our borders.
I''m pleased to be here with my counterparts from HHS, DHS, and State Department. And because we worked very closely together with them, as well as state and other federal agencies, to ensure we are well coordinated and are ready to respond, not as one agency, but as the United States government.
In fact, I''m pleased to report that USDA has accomplished all 48 tasks for which our department was given primary responsibility in the implementation plan to complete in one year. This involved a tremendous commitment by many people, both within Animal and Plant Health Inspection Service, where I work, and throughout USDA, from the Foreign Agriculture Service to our colleagues from Agricultural Research Service to Food Safety Inspection Service. I will certainly not attempt to review all of the areas in which we''ve made progress, but I would like to share just a few of them with you today.
APHIS''s emergency coordinators have participated in more than 50 state and county level tabletop exercises to ensure that we are ready, not only at the federal government level, but that we are working closely with our state and local officials to ensure well coordinated response.
We''ve expanded the national veterinary stockpile to attain another 40 million doses of avian influenza vaccine for birds. This brings our total supply to 140 million doses of kill vaccine to protect older birds. We also have a contract in place that will quickly give us access to another 500 million doses of live pox recombinant H5N1 vaccine to protect younger birds.
I should mention that it is impractical to attempt to vaccinate all poultry, as we''ve seen in other countries. In the event of a highly pathogenic AI detection, vaccines can be used to protect healthy birds outside the perimeter of the outbreak.
We have contracts in place and are continuing to test them to ensure delivery within 24 hours of the supplies we would need to respond to an outbreak. These include such things as personal protective gear, antivirals, AI field test kits, portable satellite communication equipment, portable vaccine shipment and storage containers, disinfectants, depopulation, decontamination and disposal service contracts.
We''ve tried to anticipate and address potential problems that might slow our ability to respond to an outbreak. For example, we recognize that in some instances, states have expressed a concern regarding the use of veterinarians working in an emergency response who are not licensed in their state. We are working to develop an emergency management assistance compact that would allow us to use veterinarians from neighboring states to work in the event of an outbreak.
Along with our partners from the Department of Interior and state wildlife agencies, we continue our comprehensive surveillance of wild birds in every North America fly zone, to ensure we have a strong early warning system in place. Between the 1st of April, 2006, and the 31st of March, 2007, we''ve tested over 84,000 wild birds and 50,000 environmental fecal samples. Since April of this year, we''ve already tested more than 5,000 wild birds and 400 fecal samples. All wild bird and environmental samples have been negative for highly pathogenic H5N1.
We are also monitoring wild birds in Russia, Greenland and Mexico as early warning if the virus approaches the U.S. in these species.
To meet the demands of 45 laboratories in the National Animal Health Laboratory Network and all 50 state wildlife agencies, APHIS conducted six avian influenza workshops to increase communication between all parties involved in wild bird surveillance. The workshops reviewed laboratory and communication protocols to ensure an effective and efficient response to high-path AI detection in wild birds. Our hope is that our international efforts will help to ensure that high-path H5N1 never reaches our borders.
I''ll mention just a few of our accomplishments on the international front. USDA personnel are part of rapid assessment and rapid response teams that are working in more than 30 countries worldwide. There are about 130 volunteers available for international deployments, either through the FAO or bilaterally between the infected country and the U.S. We also have a system in place to rapidly deploy USDA assets when needed internationally, without compromising U.S. domestic response capabilities. We''ve worked in more than 50 countries to help deliver and disseminate educational materials to prevent the spread of high-path H5N1. We have helped train more than 100,000 people in other countries, ranging from animal health workers and wildlife biologists to government policy makers.
I believe we''re making a real difference, in terms of global understanding of the virus, how to combat it, and how to protect against it. We have worked with international health organizations to ensure all priority countries have established early warning networks, an important accomplishment. They all have or are working on response plans, and all priority countries also have access to our training.
We have delivered rapid detection kits to 26 countries and have worked with international partners to ensure all priority countries have access to lab diagnostic services. In other words, every priority country has lab testing services available, either from the U.S. or an accredited lab in another region of the world.
From a veterinarian''s perspective, I can tell you that I''m very pleased we began preparing in 2005 as if the arrival of H5N1 was imminent. I believe that''s part of the reason USDA has accomplished every task for which we have held primary responsibility. Of course, I''m very pleased that H5N1 has not reached the U.S., but I can tell you this: It is with great confidence that I say that we are fully prepared to respond to a high-path H5N1 if it does reach our borders in the U.S.
If that happens, it''s important to remember a few key points. USDA has two decades of experience responding to AI, including both low-path and high-path forms of the virus. In high-path AI cases, USDA has worked aggressively to eradicate the disease and the virus from the premises. For low-path AI, USDA has worked closely with state and industry partners to put in place response and containment plans that ensure effective response to low-path AI incidents, and elimination of the virus from these premises. These plans are developed to be more efficient and effective for their state and their segment of the overall industry.
A detection of H5N1 high-path AI in birds does not signal the start of a human pandemic. USDA has clear aggressive action plans to eradicate the virus if it is detected in domestic poultry and backyard birds. We have much more advanced protection and response plans than existing countries where the virus has moved from birds to humans.
In the event of an outbreak, we have a plan in place to prevent affected poultry from entering the food supply. Having said that, it''s important to mention that fully cooking poultry kills the AI virus, so it is safe to eat properly prepared poultry.
In closing, I just want to take a moment to commend the media. Many of us who work in the animal health worry that the detection of a low-path H5N1, which we refer to at a North American strain of H5N1, would spark panic stories about the dangerous bird flu arriving in the U.S. Nothing could be further from reality. We''ve now had several detections of low-path H5N1 in both wild and domestic birds. Instead of sparking panic, the stories sounded the all-clear by presenting factual information when low-path AI is not a concern.
I know that reporters are under tremendous pressure to turn stories quickly, and I want to express our appreciation for the way you''ve handled reporting on AI.
And thank you for the opportunity to be here.
DR. VENKAYYA: Thanks, Dr. Clifford. I''d like to now turn to Admiral John Agwunobi from the Department of Health and Human Services.
ADMIRAL AGWUNOBI: Thank you, Dr. Venkayya. As many of you know, the Department of Health and Human Services -- and I should point out, especially our agencies of the Centers for Disease Control, the National Institutes for Health, and the Food and Drug Administration have worked tirelessly on this issue from the very beginning.
The waterfront of activity is so large and so broad, quite frankly, tens of hundreds, many hundreds of sub-tasks have trickled down from the tasks that are presented to you today. So I''m not going to keep -- I''m not going to have a lot of comments at this point. I''ll let your questions direct where we go. I''ll try to keep my comments a little short.
The Department of Health and Human Services, like other federal agencies here today, has been working diligently, as I''ve said, to prepare for pandemic influenza, and, quite frankly, as we have in preparing for many other public health emergencies that might arise.
Our work, like our colleagues'' here today, has been based on the President''s three strategic pillars, including, as my colleague the Ambassador mentioned, preparedness and communication, surveillance and detection, and of course, response and containment.
Now, since 2005, Congress and the people of our nation very appropriately invested and provided $5.6 billion in funds to assist HHS in mobilizing the nation to prepare for pandemic influenza, and the results are quite obvious.
For the first time ever, HHS has licensed -- and I think this was in April of this year -- a pre-pandemic vaccine that can help carry through the early months of a pandemic. Enough antiviral drugs are now stockpiled among state and federal governments for the treatment of more than 50 million Americans affected by pandemic influenza.
Communities now have a series of interim guidelines to assist them with their planning. I''m very proud of the fact that HHS helped host the pandemicflu.gov website, which is a really good resource for communities, for individuals, and indeed, for government, as we share information across the many different branches -- federal, state and local.
The therapies, of course, of our guidelines offered to the public has been the CDC''s community strategy for pandemic influenza mitigation. I just would insert here that all of our interim guidelines -- all of our guidelines are interim, and the very nature of pandemic preparedness is such that as science advances, as experience is accumulated, we will update all of these guidelines over time.
Interim advice on the use of surgical masks and respirators is now available, and several public discussions of vaccine prioritization have been held. Now, the results of these discussions will, we hope, help inform how we use vaccine, both pre-pandemic and pandemic vaccine, should the need arise.
Through a series of exercises with senior government officials and the media -- we''ve actually had sessions where we sat with our colleagues in the media at roundtables and discussed what we would do under different scenarios, a better understanding of how government interacts with the media, and how media interacts with government in a crisis resulted.
HHS has worked to explain the importance of pandemic preparedness at the global level -- our colleagues at the Department of State -- but also at the local level, as we work with local leaders and how they interact with their populations. We''ve released a series of radio and television public service announcements to help better inform citizens and individuals.
There is still additional work that needs to be done, and I''ll close by saying, today we present, I think, a summary of the activities that are ongoing, almost the tip of the iceberg. So much more on a daily basis is happening, I think in every agency of the federal government, as we assure a nation prepared for the next pandemic.
DR. VENKAYYA: Thanks, Dr. Agwunobi.
I''d like to now turn to Dr. Jeff Runge, from the Department of Homeland Security.
Jeff.
DR. RUNGE: Thanks, Dr. Venkayya.
Good afternoon. I''m actually very thrilled to be up here with this group that we have been in lockstep and lock-armed with since the President announced this as a major priority. And I''d be remiss if I didn''t point out that there are others in the room, sitting in the audience, who have actually been here with us every step of the way -- the Department of Transportation, Interior, Defense, the Vice President''s Office. This truly has been a remarkable effort, in the true spirit of the Department of Homeland Security, and the integration of all these players has been really rewarding for me, personally, and for Secretary Chertoff.
In addition, there are other partners, which we understand have a big stake in this -- police, fire, EMS, emergency management, and especially the private sector -- both the medical private sector and non-medical private sector.
DHS has been focused on several major areas of activity; first of all, in supporting our sister agencies, particular USDA and HHS, to ensure their success in the event of an avian outbreak or a pandemic. But in addition, we have the unique responsibility of the protection of our nation''s critical infrastructures. I don''t hesitate to remind you that 85 percent of those critical infrastructures are privately owned and, therefore, depend on the investment of both time and resources of the private sector.
We are focused on management of our nation''s borders, and especially management of the overall incident, if the institutions of the United States are threatened by a high-category pandemic, including integrated bio-surveillance, planning and exercising our plans for incident management. Maintaining domestic security and civil order falls within our bailiwick, as well as assisting in providing mass care and coordination of federal resources in the event of a high-category pandemic, as well.
Some highlights also that I will just toss out to you is that our incident management planning team has completed work on the Federal Con-Plan -- the concept plan which pulls in all of the federal agencies'' plans and turns them into a single document from which other operational plans will be cascading. Our critical infrastructure partnership division published a critical infrastructure and key resource guide last July to help our private sector critical infrastructure partners to figure out what they need to do in order to make sure that they are able to function in the event of pandemic.
In so doing, our private sector office and policy -- and our Critical Infrastructure Protection Office have conducted over 100 symposia around the country with the private sector, large and small businesses, EMS, state, local officials, police and fire. In May, DHS released the 17 all-hazards sector-specific plans as part of the National Infrastructure Protection Plan, which systematizes the ability of critical infrastructure to maintain their business operations.
Currently, the Office of Health Affairs is coordinating the incident management planning teams'' border management policy with our components and with the interagency involved, especially many of the individuals who will be involved will be state and local health officials -- I''m pleased to see Dr. Jaris here from ASTHA -- State and Territory Health official -- who are assisting us with this border management thinking.
CBP -- Customs Border Protection -- is coordinating with Canada and Mexico on trilateral border preparedness. We have developing guidelines and best practices for law enforcement, EMS, public works, and emergency management through a series of conferences. And TSA is leading a group of officials from CBP, the CDC, State Department, DOD and FAA to develop a plan for the management of the nation''s commercial aviation system in the event of a pandemic.
But a few things that the department is involved with -- I would like to echo Dr. Venkayya''s comment that these activities, though they are intended for the mitigation of a human influenza pandemic, will indeed provide the structure to deal with any other biological threat, whether natural or an instrument of terrorism. We at DHS are focused on multi-use institutions that we can put into place for whatever emergencies arise.
So with that, I''ll turn it back over to Dr. Venkayya. Thanks.
Q: My question is for Dr. Venkayya. And I guess I''ll start with, thanks for this briefing, and also thank you for setting I think an incredibly important example of government accountability. You set out a series of tasks and you dutifully reported on them. And I think that''s a model for how public health should be done and how government should work in general.
My question for you is, as we learn more about what it takes to respond to a pandemic -- and I''m sure there will be some groans from some of agency people here -- will you be adding tasks to this implementation strategy that will reflect that changing knowledge and some of the new efforts you''ve undertaken? And the example that immediately springs to mind is the community mitigation guidance identified a whole series of things that the federal government and state and local governments need to be doing to make those real, and so will there be revisions to the underlying document that reflects those additional tasks?
DR. VENKAYYA: Thank you. Just to recap in case anyone didn''t hear that, the question is, given the evolving nature of the threat, our understanding of the threat, and the advancements that we have in various areas, some versus others, will we be amending the implementation plan?
We actually, when we released the implementation plan, in the front of that document, tried to address your point. And I''m going to reaffirm that, and that is that it is a living document and we know much more about this virus; we also know much more about what we need to do to enhance our all hazards preparedness now than we did when that document came out. And so we have revised actions as we''ve gone forward.
Just to give you a couple of examples: There are 14 actions that have been postponed this time around. The last time, back in December, we postponed, I think, 12 actions that were related to community mitigation guidance because we knew that because of additional consultation, those actions couldn''t be completed until we released the guidance in February. And we''ve now gone and worked toward getting those done. I think most of those, if not all, are done.
A similar situation with those 14 -- we''ve actually worked with, in the case of the border and transportation actions, we''ve worked with DHS to bundle actions together so that we can check the box on multiple actions with a handful of activities.
As far as adding to the list, I will tell you that that implementation plan represents just a small fraction of the activities around government that are going on in the name of pandemic preparedness. As Admiral Agwunobi alluded to, in the case -- he didn''t say this explicitly, but CDC, for instance, has over a thousand actions that they''re undertaking in the name of -- and I believe they''re all connected to pandemic preparedness. It''s remarkable. And I think that that''s -- while that may be an extreme example, I think that''s the case at every federal department and agency.
We want to be careful about balancing the burden that we place on agencies with reporting requirements and so on, by adding to the implementation plan and the need to get the work done. And so we''re using a variety of vehicles to get these other things, to move the ball forward in these other areas. And those fall into our traditional policy process, which does have taskings and does have deliverables. We don''t report on them in the same manner, but we are ensuring accountability within the government.
Q: I guess just as a follow-up, my plea would be that, without creating a huge burden, as we identify some of these additional tasks -- I mean, the beauty of this is that there is a way for the public and for everyone who is concerned about this issue to really know -- to monitor the progress that is happening. And while there may be other vehicles that work internally to the government for you to monitor what is happening, it''s much harder for the government to do that monitoring.
DR. VENKAYYA: Point taken. Thank you.
Q: There''s a couple things going on in the financial services sector about addressing if there''s a pandemic -- a work-at-home strategy. And we''re working with NCS and doing some modeling there. I think the model is, we know it''s going to happen, there''s not going to be enough bandwidth to work at home because everybody is going to be working at home, and kids are going to be at home downloading stuff and there''s not going to be enough bandwidth there. We''re also doing some studies -- actually, a whole exercise in the fall -- I believe a few hundred, maybe even a few thousand institutions participate, financial institutions, and doing a series of injects over a three-week period. I think Treasury is helping fund that.
But your thoughts in general about maybe a national policy, if this does hit, can there be ways to actually restrict bandwidth or usage of that bandwidth to critical infrastructures, so there isn''t gaming and other things going on and using all the bandwidth out there?
DR. RUNGE: That''s a great comment. Thank you very much for bringing this up. As groups like yours begin to engage -- and we affectionately call that the last-mile task force, because the concern is that the last mile of telecom is really the most vulnerable piece of this. Unbeknownst to me as a physician, but working with NTIA and the Department of Commerce and your group and others -- Secretary Chertoff has actually asked the question to us recently, what additional authorities should we have in place in the event of a pandemic that we may not have now. Our general counsel is looking at this issue, particularly the issue that you raised about the large proportion of our vital bandwidth is consumed by playing video games over the Internet. If the technology exists, there may be some development of compatible authorities in order to deal with that.
Q: I''m an emergency physician and health care practitioner. I think that clearly, the efforts made by government and others have been very admirable, and the coordination and collaboration both domestically and internationally is truly impressive. However, at the same time, domestically, our health care system is quite taxed, particularly if you look at emergency departments you''ll see that the latest CDC statistics out just a couple of weeks ago show greater than 115 million visits in the last year.
So in a period where you have increased demand, increased need from folks who are ill, some of them quite seriously ill, I''d like to hear more how you''re going to address two components -- one is, how we''re going to educate the public to not overtax the system unless it''s really necessary; and two, how we''re going to help particular the private sector deal with the dramatic increase in demand at a point where we''re already close to being maxed out?
ADMIRAL AGWUNOBI: My boss, Secretary Michael Leavitt, has often expressed that his main concern is our ability to prepare and maintain the surge capacity in our health system, a capacity to surge up to the increased demands that we might see in a pandemic. Obviously there''s another part to that, and that is to recover and get back to its baseline after a pandemic has passed.
With that in mind, a lot of work has gone on. When the Secretary makes it a priority and when the administration makes it a priority, you can well imagine that it becomes something that we''re all very engaged in. A series of activities are ongoing today with a view to trying to adequately define what the gaps might be under the different pandemic scenarios, where they might be. All too often we talk about ventilators, which is an important part of the equation, but there are other issues that go into the care of the critically ill associated with a pandemic, to speak of everyone else who have ongoing health care needs, as well.
A series of discussions are underway to try and better define what the gap is, and then to define how we might sequentially and incrementally fill in those gaps over time. I think it''s appropriate that I also add that the solution to your specific questions isn''t just a federal responsibility. I mean, very clearly, each community, each state, each locality needs to engage in discussing what the unique needs are. And the reason I say that is because we don''t have a uniform system across every state, across every community of our nation. No two communities and their health care assets are exactly the same.
It''s also true that no two communities, in terms of their populations, are exactly the same. The challenge in communicating with populations is always, how do you do it in a language and in a format that is accessible to the community that you''re speaking to -- African Americans in an inner-city region, for example, rural settings, and others. So these are all important considerations.
We have released the community planning guide for providing mass medical care with scarce resources. It''s a tool that we''ve provided to the public and to health care providers to help them begin thinking through the roles that they might play in this partnership of preparing our health systems. As we reach out to our public in a pandemic, I have no doubt that they will -- that we''ll have to give them guidance on triage, on what to -- on where to take less emergent needs, and on when to present to the health system. And we''re very proud of the work that HRSAA -- our Health Resources and Services Administration Agency -- and CDC have been doing in trying to define how that might play out in a natural pandemic.
I''ll end by saying there''s no cookie-cutter solution to this. There are many variables that are critically important to the final solution, not the least of which being what kind of pandemic are we dealing with. The advice that we give to the public, whether it be antiviral use or potentially vaccine use, and prioritization, for example, and indeed, the triage question about how to access and when to access health care, might differ greatly depending on whether or not it''s a category one, a mild pandemic that might look more like a seasonal flu, with perhaps the elderly being more affected than anyone else -- the advice that we''d give a community under that circumstance might be very different than, say, a category five pandemic like 1918, where perhaps there might be excess mortality in the young and robust, a very different scenario that would require a very different intervention.
I think we''ve stunned them. (Laughter.)
Q: The 1918 flu, going back and reading some of the books about that, the school systems in Philadelphia, they didn''t close those right away and they had a higher death rate, for instance, than in St. Louis or Minneapolis and some of the other cities where immediately they took action to close the schools. But then if they reopened real early, then the death rate went back up. Is it going to be local jurisdictions that will close the schools -- because that seems to be where most of it is transmitted -- or is it going to be a national -- will national authorities have the ability to actually do that, or what?
ADMIRAL AGWUNOBI: We''re smiling because there''s been a lot of discussion internally and with our stakeholders on this subject. Today, we continue to believe that the front line of the fight against a pandemic will be fought locally. Local leadership and local communities are going to have to step up and lead. And that''s including making decisions based on the existing infrastructure of our education system, which is local.
Having said that, we believe strongly that a coordinated approach across the nation will be much more successful than one that is not coordinated. And as you can well imagine, the CDC, Department of Homeland Security -- I mean, there are work force implications that relate to school closures, as you can well imagine, consequences, and indeed, Homeland Security and others will all be engaged in, number one, making sure we educate local leaders in no unclear terms as to the need to have plans that they can implement in an emergency; exercised plans so that they''ve worked out the kinks; and of the importance of doing so in a coordinated fashion.
Now, I don''t want to leave you with the impression that a pandemic will hit all at once across the entire nation simultaneously and everybody will be asked to close their schools on the same day. It doesn''t work that way, as all of you know in the stakeholder community, pandemics roll through communities in a somewhat unpredictable way. So the coordination that we''re talking about are a set of key epidemiological triggers that we''d urge everyone to build into their plans and that they activate their school closures -- actually, their non-pharmaceutical interventions, the many non-pharmaceutical interventions that might be out there, that they would activate them in some coordinated fashion linked to those key epidemiological triggers.
When you look at the epidemiology waves in disease, there''s a right time and perhaps a wrong time to intervene with different interventions. Our hope would be that we could get everybody to the point where they''re pulling the trigger based on the same coordinated set of findings. I don''t know if, Rajeev, you want to add to that in some way.
DR. VENKAYYA: Well, I know that Jeff at DHS has also thought a lot about this. We have great concern that in an eventuality like this, where the authority does reside at the local or state level, that you could have a patchwork implementation approach and have, say, a community on one side of the state line behave -- or one county behave one way, and the next county over behave differently.
And I think it''s critically important for the federal government to provide that clear, unambiguous guidance early -- revised as needed, but provide that early so that communities know exactly what they''re on the hook -- what the federal guidance is. And if they''re not going to follow federal guidance, they probably ought to have a good explanation for their populations, because this is -- these are, essentially, potentially life-saving interventions. And so if a community wants to deviate from that guidance in order to preserve something else, then I think that they''re going to owe an explanation to their populations.
ADMIRAL AGWUNOBI: I''ll just add one last point on this. The issue about community mitigation is that it has to be linked to data. As I''ve said, the epidemiological curve locally. And the first people that know what''s happening in their community, in terms of illness and disease, are local public health providers. And it is just -- it''s much more expedient to put key decisions in their hands -- when you first see these events, act in this way. That would be the kind of guidance we would give them. It''s a faster way to get things done, rather than trying to roll the data together and then send the action back down from through some central point, which delays an intervention.
Q: Each of the departments here and the agencies within have a role in detection, so coming from public health labs, it''s really the focus of my concern. What mechanisms does the government have to coordinate, in terms of the detection? When we seem the implementation plan, there won''t be any announcement of a pandemic until we know what actually is out there. So detection is pretty important.
ADMIRAL AGWUNOBI: I''m going to try and take a stab at the question. Let me just make sure I understand. Your question is how do we propose to coordinate the activity of the local labs?
Q: No, how are you coordinating the role of detection within each of the various departments? Because it could be detection through -- in human or avian or it could be overseas.
DR. RUNGE: One of the action items -- which unfortunately says "in progress" because we have not completed it yet -- is the standing up of the national biosurveillance integration system at DHS, which is actually a commonly owned partnership of HHS, CDC, HHS-FDA, Dr. Agwunobi and the Secretary''s office, USDA, Interior, Defense and Department of State and Department of Transportation is currently a signatory, this is -- we are building a system which will integrate the various data systems that the USDA has for monitoring things like the health of flocks in states, the biodefense that is operated by the CDC. There are several states have their own syndrome, so they want systems. We have access to information coming in from the National Infrastructure Coordinating Center, from the private sector, who report issues within their sectors. We are exploring partnerships with private sector companies that gather data on what drugs are flying off the shelves of pharmacies.
So this is an effort that we have promised to the Secretary by September 2008, to get it completely delivered. It''s very clear that all -- that state and local, federal government, as well as the private sector have information out there that is currently not linked and is somewhat stovepiped. This is an effort, in fact, to put that together and to integrate this. This is a presidential directive under Homeland Security Presidential Directive, both 9 and 10, for biodefense and for food defense. So we are sending that up. It''s taking a while; there are some technology challenges, as well as some challenges with coordination. But we take that very seriously.
And, by the way, the laboratories are very much a part of this, as well. They will report up through the HHS channel, we believe.
AMBASSADOR AGWUNOBI: On the purely human disease front, CDC is acting aggressively to enhance and improve its influenza surveillance system, which is a collaboration of hospitals and providers, up through states and collaborating directly into CDC on influenza and influenza-like illness. That system is being enhanced; there is an ongoing project to try and expand the numbers of sentinel reporters that are out there across not just, quite frankly, domestically, but, indeed, a big part of our international work has been about broadening our view in terms of surveillance in other countries around the world.
So there is a lot of work on the human disease front, as well, in that regard.
Q: First of all, congratulations on all the important work that''s been done to complete the (inaudible) plan. I was just wondering in the different areas that you work in whether or not you''re seeing any preparedness fatigue, given that we''re two years into it and will probably go -- continue for a few more years before anything probably happens. But just wondering if you''ve seen any preparedness fatigue, and if you haven''t, what are your thoughts about how you should deal with it, once it starts surfacing in years to come?
DR. VENKAYYA: Well, from our perspective I think that''s absolutely the case. We hear this in every discussion about avian and pandemic influenza, and it represents a real challenge. I think people realize that this would happen eventually, that the longer you talk about something and nothing happens -- when I say "nothing," I mean an actual human pandemic -- then it becomes to have the sound of a Y2K, if you will.
And so while I think that we probably benefit from a little less hyperventilation in certain media outlets -- none of which are in this room -- (laughter) -- I think that it''s the responsibility of the government, of governments at the federal, state and local level -- leaders, if you will -- to maintain the focus. I think that one of the things that the pandemic threat has done for all of us, I mean, the global community, is it''s given us something specific to focus our preparedness efforts on. And it''s not something made up, it''s a very real threat. And that has done more to put wind in our sails to advance these preparedness activities.
If you look at the implementation plan, though, you''ll find that there are largely -- the majority of actions there are generic. They are all hazards, or at least all biohazards in nature. There are very few H5N1-specific taskings in there. And so we have made a concerted effort to get that message out there, that this is going to be a long journey that we''re -- irrespective of what happens with this one virus, we are enhancing preparedness in ways, and using coordination systems that we never would have envisioned two years ago if we were talking about preparedness for, say, anthrax or smallpox.
So I think it''s that message that we need to get out there about all hazards preparedness and the need for leaders to keep their eye on the ball. I don''t know if my colleagues want to add anything to that?
ADMIRAL AGWUNOBI: I would concur completely. I think especially when you begin to translate what you''re seeing here today down through federal government to state government and then down to local governments, where the tactical person in the trenches is all too often the same person -- a community nurse who is educating people on pandemic influenza, on bioterrorism, on other issues -- and, yes, at some point there might be exhaustion in that workforce.
But I agree with Dr. Venkayya, with Rajeev, that the solution is absolutely about translating this, as we have these conversations, away from the notion of some acute threat today to this larger sense that we have to be prepared forever against many different bio threats, H5N1 being one -- there will be others in the future. I was in a conversation yesterday with Dr. Webster at another setting and it was quite clear that I think we need to recognize that if H5N1 were to disappear tomorrow, the need to be prepared for a pandemic which still exists, and this need to be prepared is something we own as a community, as a society, for the long run.
And so we do have to, once we get past that peak, get to a decent plateau of sustained commitment and sustained resources and a sustained approach to this.
DR. RUNGE: I would totally agree. And I appreciate you pointing this out. And this is -- and John is right about this, that, you know, we need to reach a battle rhythm of a state of preparedness that is higher than it was before the President made this a priority, and the absence of any hyperventilation but more as a marathon.
There''s another piece to this, and that is that we''ve asked the private sector to pay for, to invest in preparedness. And the businesses that have come forth to do this understand -- they want to stay in business regardless of what ill befalls them -- if it''s a pandemic, if it is another biological attack, natural or manmade, they need to have these institutions in place. And they have really stepped up to the plate and provided a significant amount of investment to do that. We are dependent on their goodwill, on their patriotism for doing so.
And I''d like to point out one last thing, and Rajeev mentioned Y2K. I was practicing medicine in North Carolina when we turned to the millennium. The year before, every lab slip came down from the lab on a piece of paper with a runner, I had an aging PC on my desk, the hospital mainframe was a 1979 Burroughs that had to have five guys constantly maintaining it. On January 2, 2000, I had access to my patients x-rays, I could do quality assurance from my PC, laboratory results were automated. There was no question that the investment in Y2K improved the situation in health care. I''m hoping that the investments that are country is making in vaccine technology and in revamping the public health system to deal with this will actually pay dividends if we never have a pandemic.
ADMIRAL AGWUNOBI: We''ve just invested, as all of us know, a billion dollars in looking for new ways to produce vaccines that will benefit broader health care and public health interventions.
DR. VENKAYYA: I think Ambassador Lange and Clifford want to make a comment, as well.
AMBASSADOR LANGE: I just wanted to mention a bit about the international side of this. There is certainly less overall media attention to this, but governments are still engaged. And what we''ve found is that governments in countries that are experiencing avian influenza in the poultry populations are very much engaged in this. There was a meeting in Sydney, Australia, several weeks ago with health ministers from the Asia Pacific Economic Cooperation forum. And they spent three days together and almost the entire subject matter was avian influenza and planning for a possible pandemic. And they discussed some of the economic and trade ramifications of a pandemic, et cetera, et cetera.
But, of course, that''s the region of the world where this began. You can look at West Africa these days and it''s spreading there. You can look at some European countries who have just encountered recurrences. And the countries that have experienced the avian influenza, in general, have a little more focus on this as a concern.
But the other side of it is that governments as a whole are very engaged, even if there''s less media coverage. And we''ve had continued high attendance at this major international meetings that I listed in my initial statement, and all indications are the government of India is very engaged to have another big attendance at its meeting in December.
DR. CLIFFORD: I just wanted to comment from the Department of Agriculture, relative to the question of fatigue. I think we all recognize some degree of that. But I think the benefits of this type of planning, as well as other planning, it''s greater reliability on one another, greater partnerships with the industry and the states in trying to do these things in a partnership way versus individually. In years past, you know, the Department of Agriculture and the state departments of agriculture may have tried to go do these things alone.
We don''t do that anymore. We do it together. And that helps address some of these issues of fatigue, as well as capacity building to handle bigger events.
Q: I want to -- as Dr. Jeff said also, I think this is an excellent example of putting something out there, doing a task and being held accountable for it. And we all have lessons to learn here.
One of the other areas which I think guidance could help us at the federal level is with actual distribution of antivirals. Every state has its own medical board, its own rules, who can prescribe under what conditions, and it''s going to be very difficult to get this on a state-by-state basis and have it consistent.
In addition, we see now the private sector stockpiling, as well as the public sector. So addressing those issues of, should a pandemic hit at a certain level, what would be an acceptable guidance for how to distribute? For example, how necessary would it really be to see a physician? (Inaudible) the value of a history in the face of a pandemic (inaudible). And we certainly know, as the gentleman said back there, the clinical system simply couldn''t handle it if people were required to see their physicians. So guidance around that would help us break down a lot of barriers and walls, as well as bring all these medical boards into line.
ADMIRAL AGWUNOBI: I take your comment very seriously. I think it''s an important aspect of the work that we need to do going forward. I think we should do it in partnership with the states. I mean, very clearly you want to build in the unique nuances that exist in every state because, if not, you holler "evacuate," and some can and some can''t, if you catch my drift. I think it''s important that we do it in partnership with states.
Q: I think in partnership, and that''s why guidance is the key word here.
DR. VENKAYYA: Yes, and I would echo what Dr. Agwunobi said, and as you know, this is a distribution of countermeasures, whether it be in response to a bioterrorism event or in the unique circumstances presented by a pandemic -- I should say the different circumstances presented by a pandemic is one of our greatest concerns. And we get back to this issue of heterogeneous capabilities across the nation. And to the extent that we can put best practices out there as to how to accomplish this in a manner that minimizes the burden on the public health and medical system, I think that''s, frankly, the federal government''s responsibility to do that.
On the issue of use of antivirals in new ways based on data -- things like use of prophylaxis and stockpiling by businesses. I know the Department of Health and Human Services and CDC -- and I think you''re aware of this -- are working hard to develop guidance along those lines that reflect our current understanding based on recent evidence on what prophylactic use of antivirals could afford with regard to overall community transmission. So that''s in the works.
Q: If I could, just one more follow-up. The other place that it''s been very helpful is, for example, when you''re negotiating a contract with Roche for antivirals on (inaudible) that the states can (inaudible) or not. We all are, thank you. Other distributions like a FedEx, those large professional distributors might be a place for the federal government to negotiate a national contract that the states could or not opt into.
ADMIRAL AGWUNOBI: Great thoughts and ideas and I think we''ll talk about them, as well, as we move forward.
I think when all is said and done it''s going to be about collaboration -- with the private sector, with government, with different levels of government working together, with individuals, as well.
Q: My question is probably going to sound justice and law-related, and I know none of you are from the Department of Justice. But I guess one of my concerns -- and I think it is a good thing that you''re talking about guidance from the federal government, I think that''s what my members look to for the federal government to be able to provide. But at the same time I guess I''m concerned about, is anyone looking at state constitutions or laws and what is permissible? And the reason I ask it is, let''s say the guidance came down and it said departments of health in every state should close down the schools at such and such a point. Well, what if you do that and five states say, not a problem -- and 45 states say, my constitution, my statute prohibits that. There is no authority for my department of health to take that kind of action.
And I guess my question is, to be a little bit more preventative from that happening, is there any research or anybody taking a look at some of that, so that we don''t get too far down the path and then suddenly discover, oops -- and we''ll have to rely on collaboration, which is great, but in a time of crisis it would be nice, maybe, if we had thought that through before we get to that point.
ADMIRAL AGWUNOBI: I''ll just say that the collaboration that I was referring to is ahead of time. A collaboration in reviewing where we might go and what the barriers might be and what the potential solutions those barriers might be. I''m very proud to work with (inaudible) and I ask the association of state and territorial health officers. We work closely together now on the public health questions and the public health challenges trying to figure out if we have the public health guidance, what might the barriers be at the individual state level to implementing that guidance.
I don''t know if we''re doing something similar in the business aspects and the infrastructure aspects. I think we are working with states to try and figure out where might the barriers be so that we can design work around or work-overs, depending on what the issue might be.
DR. RUNGE: I think that part of the concern here may be addressed by the public dissemination of the guidance and the notice and comment that will come with some of the actions that HHS and the U.S. government are taking. We would hope that through that process we would find out that there are barriers that exist with the recommendations.
AMBASSADOR LANGE: There has been -- I know that CDC has worked, I think with Hopkins, to survey state authorities, in the case of school closure, to examine whether that resides at the local level or the state level, and where it pivots, in some cases, in the case of a crisis. And I think that they -- the last report I heard on this was that they had found -- they had identified at least a level in all 50 states, they knew where it was as of today, but it was clear that there were some states that needed to do some work to figure out what you do in an actual crisis.
So I think attention has been drawn in that case for states to the issue, but I''m certain that there are other authorities issues that we still need to explore.
ADMIRAL AGWUNOBI: Prescription is one of them, the rules and regulations regarding prescriptions -- who can do it and who can''t, and under what circumstances does that change. Those typically are set by boards of health at the state level. So as we issue guidance we have to go into discussion with them to try and figure out where might the barriers be, how many states could come along with this guidance and how many other states would have to have some emergency authority that they''d use to be able to comply with the guidance.
That''s the purpose of having the conversations now, so that we can work through those issues before a pandemic ever occurs.
Q: Looking at the report and what you said, it sounds like the really big, hard part is still ahead of us, though -- having the diagnostics in place, having the surveillance in place, having the vaccines that we need. Would that be a correct characterization?
DR. VENKAYYA: I think it''s fair to say that the things that we have called out as being activities that we need to continue to focus attention on, where essentially we''re not there yet, yes, those are some very difficult tasks. I mean, the reality is, on the rapid diagnostic front, that we have done -- HHS has done a careful survey of the technological horizon to see what the near-term opportunities are, and there isn''t much there. We talk about the idea -- and this is even called out in the report -- what''s it going to take to get a 30-minute diagnostic, dip-stick test, if you will, for a pandemic virus -- that''s not going to happen tomorrow, but it''s a critical priority.
The reality is that if we have a way to target our antiviral medications more effectively, that dramatically reduces the stockpile requirements, the amount that we need to have in place.
The biosurveillance issue is -- unfortunately, we can''t flip a switch and all of a sudden have nationwide biosurveillance capability in all communities, because that really is something that has to be based upon community capabilities. And that''s going to be different in different communities.
You know, one of the -- the reason we have pushed the community mitigation guidance so hard -- when I say push, I mean worked hard as a government to try to nail down our thinking on what -- our best thinking as to what might work is because these are the hard realities, that we''re not going to be able to magically create surge capacity overnight. And so while we are continuing to work on that supply side of the equation, if you will, the medical and health personnel supply side, that we absolutely need to take advantage of any opportunity to reduce demand. And that''s where the lessons from 1918 come in.
And this is why we work very hard to force people''s thinking around what can we actually say, based on the available evidence today, recognizing that we might have to modify this further, that will allow them to begin planning. Because the reality is we''re not going to have all the answers to these questions, but people need to begin planning now. And so that is why we''ve taken that tact in the case of the community mitigation guidance.
I don''t know if my colleagues want to --
ADMIRAL AGWUNOBI: I''m not sure this is what you meant, but I wouldn''t, on the other hand, characterize the stuff that we have completed as less important than the stuff that we haven''t because that''s not the case. A lot of the work that''s been completed is critical work, especially our work at the international and, indeed, with industry and critical infrastructure -- it''s all critical work that we''ve managed to get done.
DR. VENKAYYA: I completely agree. Thank you.
Q: I can''t resist asking -- Dr. Agwunobi, last week, a former direct report of yours, Richard Carmona, released a fierce criticism of this administration''s leadership on a lot of health issues, among them global health preparedness, many others. Why was he so critical? It seems as though many of the issues he was talking about could overlap with the ones you all are talking about today. Was he right, or have you --
ADMIRAL AGWUNOBI: I''ll be candid, I don''t know why he issued those criticisms. I worked with him for at least one year, or short of one year, and saw none of the criticisms that he''s reported to have offered. I wasn''t in the hearing.
I can tell you this; that the Surgeon General''s role is a critically important one. It''s about educating the public on health and public health. He also has a role related to commanding and helping nurture the Public Health Service Commission Corps.
The role of preparing our nation for bio-terrorism and for pandemics is one that is shared across, as I''ve stated before, a number of the world''s finest agencies -- the Centers for Disease Control, with Julie Gerberding, NIH with Elias Zerhouni, FDA, Andy bon Eschenbach. And if there''s one thing that we are blessed with in this federal government, it''s experts, it''s leadership, it''s people that work together collaboratively to get the job done.
Today -- and this report is evidence of it -- I''m proud to say we get the work done. I''m not quite sure where he was coming from.
DR. VENKAYYA: I want to thank everyone again, and my colleagues, for taking this time today. We had four departments on the stage here. There were many, many other departments. There are 15, actually, departments called out as lead agencies in the national implementation plan, a total of 18 agencies that are called out in total.
Actually, I think one, in particular, deserves to be acknowledged, and that''s the U.S. Agency for International Development -- USAID -- which is within the Department of State, but is essentially managing the investment portfolio for our investment activities. And Ambassador Lange did a very nice job of speaking to their activities, but I think that it''s important to acknowledge their efforts -- but also, Departments of Labor, and Commerce, and Education, and Transportation, and Interior, and Defense -- and the list goes on and on -- Veterans Affairs -- I''m going to stop because I know I''m going to forget some. It''s always a mistake. (Laughter.)
So I just want to highlight that this has been a cross-government effort. And the coordination systems that we have developed here within the federal government we really think need to be replicated at the state and local level. And so we hope that we can translate the lessons that we''ve learned in the federal government about cutting through the silo of mentality that exists in any bureaucracy to accomplish that coordination before an event occurs -- to the extent that we can advance that, we want to.
I also want to highlight the importance that we now appreciate of engaging entities outside of government -- the private sector, non-governmental organizations, and individual, themselves. Folks in government -- Secretary Leavitt, Secretary Chertoff and others have said time and time again, if and when a pandemic occurs, individuals and communities are going to be largely -- going to have to use resources at their disposal to make their way through it. I think that that''s an important message, but I think that that message absolutely must be accompanied by very clear and explicit guidance as to what steps those communities can and should take in order to prepare themselves.
The federal government I think is in -- we believe is in the best position to develop that guidance. You will see a tremendous volume of that guidance that has emerged over the course of the past year that is now available on pandemicflu.gov, created by the departments and agencies that you see here on the stage. And actually, a number of federal participants are in the audience right now from those agencies that I mentioned.
And so the challenge now is translating that guidance into actual action at the state and local level. And so that, I think, is the challenge we face going forward. And we do appreciate your time and continued attention to the issue. (Applause.)
END 2:22 P.M. EDT
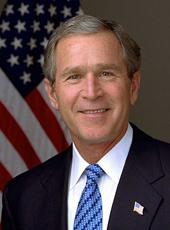
George W. Bush, Press Briefing on National Strategy for Pandemic Influenza Implementation Plan One Year Summary Online by Gerhard Peters and John T. Woolley, The American Presidency Project https://www.presidency.ucsb.edu/node/276116

